DRUG-RESISTANT SUPERBUG SPREADING IN HOSPITALS: STUDY
IN NEWS
A superbug resistant to all known antibiotics that can cause “severe” infections or even death is spreading undetected through hospital wards across the world, scientists in Australia warned on Monday.
The bacteria, known as Staphylococcus epidermidis, are related to the better-known and more deadly MRSA superbug.
It’s found naturally on human skin and most commonly infects the elderly or patients who have had prosthetic materials implanted, such as catheters and joint replacements.
Study, published in the journal Nature Microbiology, showed the need for better understanding of how infections spread.
Another Australian study, published last month, suggested some hospital superbugs are growing increasingly tolerant to alcohol-based disinfectants found in hand washes and sanitisers used on hospital wards.
What is superbug?
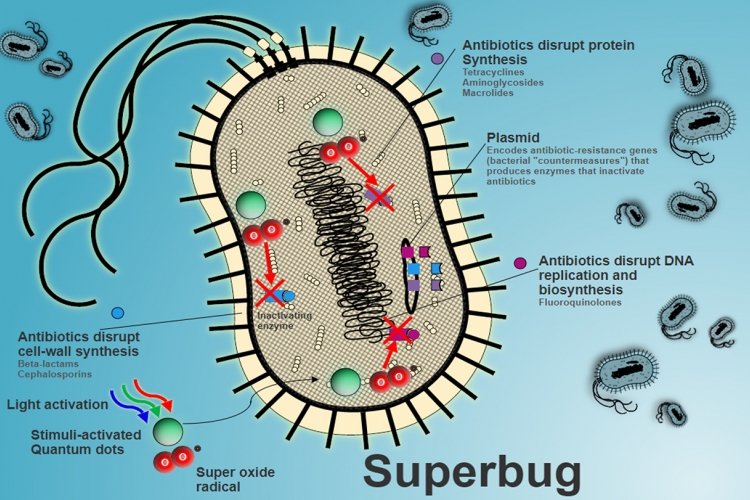
Superbugs are bacteria that have acquired resistance to several types of antibiotic drugs either through genetic mutation or through build up of resistance over time. That is, antibiotics will have no effect on such bacteria.
What are antibiotics?
Antibiotics are commonly prescribed drugs that treat bacterial infections such as diarrhoea and bacterial pneumonia. Antibiotics also prevent infection of surgical wounds. The drugs act on the disease-causing bacteria in our body by either killing them or inhibiting their growth. Antibiotics are among the most commonly prescribed drugs for people. They’re also administered to livestock for disease treatment and prevention. Antibiotics revolutionised modern medicine in the 20th century.
Who invented the first antibiotic?
The first antibiotic, penicillin, was discovered by Alexander Fleming in 1928. Fleming was recognised for the discovery in 1945, when he received the Nobel Prize for Physiology or Medicine, along with Australian pathologist Howard Walter Florey and German-born British biochemist Ernst Boris Chain, both of whom isolated and purified penicillin.
What led to the development of antibiotic resistance?
There are multiple factors that led to the increase in antibiotic resistance among bacteria.
- Bacteria are living organisms and they evolve, adapting to new environments and new challenges, just like any other organism.
- The trait of antibiotic resistance develops over time.
- Bacteria share genes with other bacteria and thus pass on the resistance.
- Bacteria strong enough to survive a drug will have a chance to grow and multiply.
- While antibiotic resistance occurs naturally, misuse of antibiotics in humans and animals is accelerating the process.
- Unnecessary prescription by physicians or self-medication by patients: If an antibiotic is taken against a viral infection, the drug does not target the disease-causing virus but instead kills the good bacteria that aid in digestion and in fighting infection.
- Improper disposal of medical waste leads to contamination of water and soil where the bacteria acquire resistance.
Why is this cause for concern?
Antibiotic resistance is rising to dangerously high levels in all parts of the world. Soumya Swamination, Deputy Director-General for Programmes (DDP) at the World Health Organisation (WHO), states in an article that more than 50 per cent of some groups of bacteria are resistant to almost all the antibiotics we have. We may soon not be able to treat even common infections.
How can we prevent the spread of superbugs?
We can slow the spread of the superbugs by taking antibiotics properly and only when needed.
- Only use antibiotics when prescribed by a certified health professional.
- Never demand antibiotics if your health worker says you don’t need them.
- Never share or use leftover antibiotics.
- Physicians should prescribe and dispense antibiotics only when they are needed, according to current guidelines.

 IAS -2025 Prelims Combined Mains Batch - III Starts - 14-04-2024
IAS -2025 Prelims Combined Mains Batch - III Starts - 14-04-2024